Framingham Risk Score Calculator Pdf Printer
Introduction The process of that leads to CVD is difficult to diagnose easily, prior to the occurrence of significant clinical events such as CVD-related death,. Epidemiological studies, such as the Framingham in the USA, have identified a large number of CVD risk factors which can be divided into the principal non-modifiable CVD risk factors, such as age and gender, and modifiable risk factors, including smoking, presence of and ratio of total to. The significance of these principal risk factors has been confirmed in worldwide epidemiological cohort studies, including in the UK.
Vascular Risk Reduction Resources. In addition, some components of dementia share common causal links with vascular diseases. 0% of Canadians have one or more common vascular risk factors. Most vascular risk factors are preventable or controllable and, despite the availability of proven treatments, control. Risk Score Calculator. Training & Presentations; Coding FAQs; Tools; HCC Blog; Terms of Use; Legal Disclaimers; Copyright © 2004-2019 SCAN Health Plan. This Australian absolute cardiovascular disease risk calculator has been produced by the National Vascular Disease Prevention Alliance (NVDPA) for the information of health professionals. The calculations are based on the recommendations in the Guidelines for the assessment of absolute cardiovascular disease risk. These guidelines are available on all NVDPA member websites.
The cohort studies can be used to devise risk tools that calculate the risk of a CVD event prospectively over a defined period of time, for example a decade. While the basic set of CVD risk factors is well established, numerous groups have proposed the addition of other CVD risk factors, such as, ethnicity, of premature CVD or markers of, to improve the performance of the risk tools, particularly in subgroups. The previous NICE guideline on modification and CVD risk assessment (CG67) recommended the use of a risk assessment tool derived from the US Framingham and Framingham Offspring studies to assess CVD risk. Multiple different risk assessment tools have been derived from the Framingham study, and the Anderson (1991) tool was chosen., The GDG suggested a number of adjustments to the equation to improve estimation of risk, particularly in people from minority ethnic groups. During the validation phase of the guideline, the first paper describing the development and internal validation of QRISK was published and the guideline group considered it alongside Framingham. QRISK was derived from patient records in a large UK primary care database. The GDG view was that it was premature at that time to recommend QRISK.
A summary GDG discussion is summarised in. Following publication of further literature validating QRISK, NICE withdrew advice about which risk assessment tool to use in February 2010. In this update, the GDG were asked to consider whether they could recommend one tool for assessment of CVD risk. Risk assessment of CVD has relevance for the use of modification drugs, but is also relevant to the NICE guideline (CG127) which cross-refers to this guideline and recommends for mild hypertension on the basis of overall CVD risk.
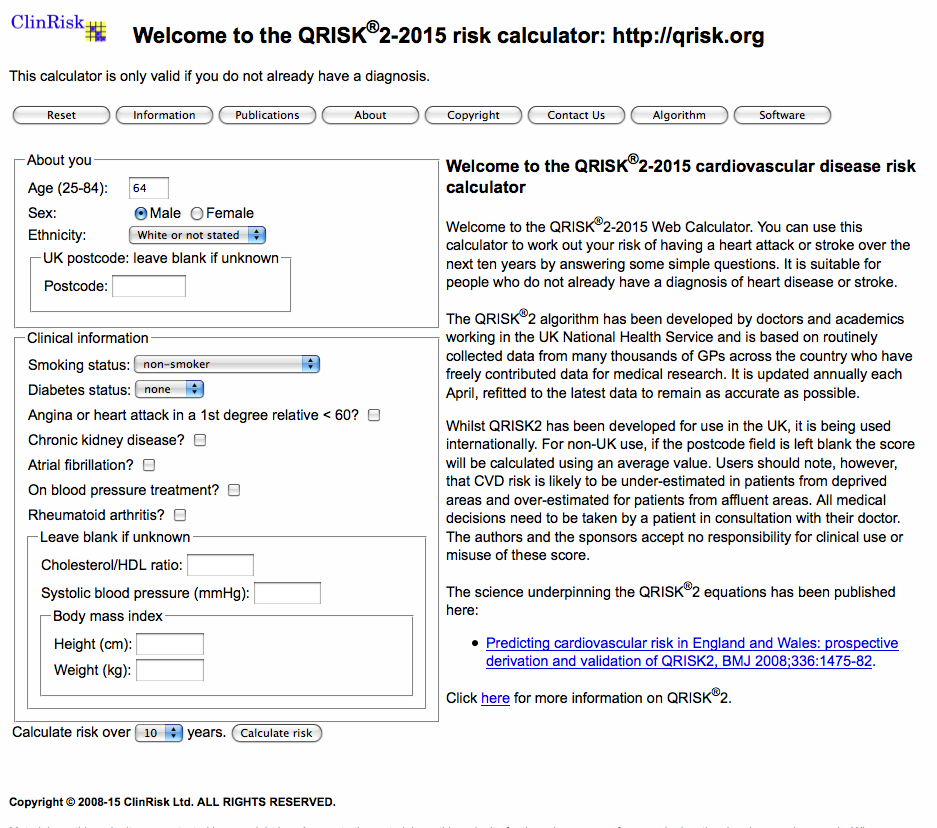
The scope for this guideline includes populations with type 1 and and people with CKD. The scope also includes consideration of risk assessment in people from black and minority ethnic groups, people with a of CVD, people from low socioeconomic groups, people older than 75, women, people with and people with serious mental illness. The GDG requested that information on age alone as an indicator of risk be reported alongside the review on risk tools. Age is the principal determinant of risk and has the potential to be a simple way of considering who might benefit from preventative. Clinical evidence We have only included tools which have been validated in England and Wales (QRISK2, Framingham and UKPDS). Data on age alone were also extracted where available. QRISK2 and Framingham are 2 online risk assessment tools for estimating the 10-year risk of having a CV event, for people who do not already have disease.
The definition of CVD is slightly different in the 2 tools. In the Framingham tool, CVD comprises coronary death, MI, coronary insufficiency, ischemic, haemorrhagic stroke, TIA, PAD, and. In the QRISK2 tool, CVD comprises CHD (angina and MI), stroke, and TIA, but not PAD). QRISK2 is available as lifetime CV risk calculator ; Framingham has also been developed as lifetime CV risk calculator, however, it is not publicly available.
UKPDS Risk Engine is a -specific risk calculator for estimating the 10-year risk of CHD (fatal and non-fatal MI, and sudden death) and (both fatal and non-fatal). The risk factors and variables included in the tools (10-year risk) are listed in. Calibration curves (Collins 2012B,) shows the calibration plots for the 3 versions of QRISK2 and the NICE version of the Framingham equation. The current version of QRISK2 and its predecessors show better agreement between the observed risk and the predicted risk grouped by 10 th of risk than does the NICE Framingham equation. All 3 versions of the QRISK2 prediction models show good calibration in all 10 ths of risk, with the exception of the highest 10 th of risk in both men and women (calibration slope, range 0.92–0.95).
The NICE Framingham equation is mis-calibrated, most noticeably for men, with a near constant over-prediction of about 5%. Calibration curves: observed versus predicted 10-year risk of CVD (from Collins 2012B). Source: from Collins 2012B BMJ 2010;340:c2442 (Ramachandran 2000,) shows the number of coronary events predicted by the Framingham model and the number observed during follow up.
The agreement is good at a predicted event rate above 30% (1.5% per year), with no significant difference between the observed and expected event rates (p=0.85). However, at lower event rates the predictive model significantly underestimates the number of observed events (p. Framingham versus QRISK2 (Hippisley-Cox 2008) Of the 112,156 patients classified as high risk (risk of ≥20% over 10 years) with the Framingham score, 46,094 (41.1%) would be reclassified at low risk with QRISK2. The 10 year observed risk among these reclassified patients was 16.6% (95% CI: 16.1% to 17.0%). Of the 78,024 patients classified at high risk with QRISK2, 11,962 (15.3%) would be reclassified as low risk with the Framingham score. The 10 year observed risk among these patients predicted to be at high risk with QRISK2 was 23.3% (95% CI: 22.2% to 24.4%). The annual rate of CV events among those with a QRISK2 score of ≥20% was 30.6 per 1000 person years (95% CI: 29.8 to 31.5) for women and 32.5 per 1000 person years (31.9 to 33.1) for men.
Both these figures are higher than the annual incidence rate for patients identified as high risk with the modified Framingham score. The annual incidence rate for these patients was 25.7 per 1000 person years (25.0 to 26.3) for women with 26.4 (26.0 to 26.8) for men.
In other words, at the 20% threshold, the population identified by QRISK2 was at higher risk of a CV event than the population identified by the Framingham score. Recommendation 8.
Use the QRISK2 risk assessment tool to assess CVD risk for the primary prevention of CVD in people up to and including age 84 years. new 2014 Relative values of different outcomes The clinical outcomes that the GDG wanted to predict were CV events, in particular CV mortality, non-fatal MI and. The GDG considered calibration, discrimination and reclassification of risk assessment tools to be important.
The GDG considered that any risk tool should accurately predict the number of individuals likely to have an event, that is it needs to be well calibrated; over- or under- prediction would lead to over- or under-, which could result in significant harm. Discrimination is important to correctly classify individuals into risk groups to inform decisions on pharmacological. The GDG noted that reclassification indices are being used in comparing the performance of different risk tools around decision thresholds. The reclassification index is the difference between people re-classified to high risk or low risk, but it can be calculated in different ways and the absolute magnitude of changes is relevant as well as the difference. There is lack of agreement on the definition of reclassification index. The clinical reclassification index, based on clinically relevant re-classification decisions should also be considered. Trade-off between clinical benefits and harms One purpose of risk assessment is to decide on suitability for.
The GDG considered that the use of an appropriate assessment tool is unlikely to harm an individual patient but were concerned that emphasis on a risk assessment tool might distract from the need to use clinical judgement to inform interpretation of the tool according to the circumstances of each individual patient. Over-prediction will result in unnecessary and, whereas under-prediction means a person would not be offered potentially preventative. The evidence indicated that all the tools considered are better than chance at predicting risk. In terms of discrimination, QRISK2 and Framingham did not show significant differences from each other. QRISK2 shows better performance in terms of calibration and reclassification than Framingham: Framingham has a constant over-prediction of about 5% while QRISK2 shows agreement between the observed risk and the predicted risk up to about 30% CV risk; 41% of people classified at high CV risk (of ≥20% over 10 years) with Framingham would be reclassified at low risk with QRISK2 while 15% of people classified at high CV risk with QRISK2 would be reclassified at low risk with Framingham. Economic considerations No relevant economic evidence was identified assessing the cost effectiveness of using different risk assessment tools or strategies.
The cost effectiveness of using different tools might vary if the resources needed to implement these tools were different – for example if one tool required more information, and if this would involve a greater number or length of appointments or a greater number of to be carried out to elicit the required information. However, that is not the case in this situation. Framingham risk assessment does require fewer pieces of information than QRISK2 (for example, it does not require ethnicity, BMI or of CVD to be recorded), however, these are risk factors which can all either be measured easily or can be elicited quickly by asking the patient. They are also factors which general practices routinely record, for example on initial registration with the, and are routinely held in electronic medical records. If this information is not recorded for an individual then the practice would usually seek to gather it at any available opportunity even if not needed immediately for the specific purpose of CV risk assessment. The use of an age-alone strategy is subject to the same consideration, as most risk factors are not needed to carry out age-alone risk assessment but would still be of interest to the practice and could be collected easily. Age-alone risk assessment would however not require the collection of a sample to measure levels, which is required for risk assessment using either QRISK2 or Framingham.
However, once a decision is made to initiate statin, a would then be needed to measure levels of and to check transaminase levels. In this case, the resource use has shifted from before to after the risk assessment, and so there is a potential for cost saving. However, that would only apply to those individuals aged old enough to qualify for consideration for statin who agree to attend a consultation to discuss this but then decline to initiate statin. Given the low costs of these that would be a very small saving. An age-alone strategy could in theory be adopted with fewer initial consultations, as all those in the relevant age groups could be informed by letter that they were recommended for. However, the GDG agreed that this would be incompatible with the requirement for clinicians to carefully discuss with people the risks and benefits of statin, to allow each individual the opportunity to consider whether they wish to receive such.
The GDG also believed that offering statin widely, without personal face-to-face contact would lead to low rates of uptake of. Such appointments also give GPs opportunities to discuss lifestyle risk factors with individuals, and to encourage additional or behaviours to reduce those risk factors. Therefore an age-alone strategy would not lead to cost savings through fewer consultations. Given that there does not appear to be any reason to expect significant differences in resource use in carrying out risk assessment, whatever risk tool or system is used, the cost effectiveness of using a risk assessment tool will therefore be related to its effectiveness in correctly predicting risk. The tool which best predicts true cardiovascular risk will minimise over- of those actually at lower risk but wrongly classified by the tool as over the threshold adopted, and minimise under- of those actually at higher risk but wrongly classified by the tool as under the threshold adopted. As the QRISK2 tool was found to perform better than Framingham tools in terms of calibration and reclassification, it would hence also be more cost effective to treat people on the basis of their QRISK2 scores than on the basis of Framingham scores. Regarding an age-alone strategy, the only effectiveness evidence available came from a simulated, which found it to be almost as effective as Framingham.
Evidence for an age-alone strategy in real world populations was not available. As noted in ‘Other considerations’ below, the largest problem with an age-alone strategy would be that people below the age threshold but at raised risk due to multiple other risk factors would not receive despite it being clinically beneficial and cost effective for them to do so. Thus an age-alone strategy would be expected to be less cost effective overall than using the QRISK2 tool. A potential combination of an age-alone strategy above an age threshold and a risk assessment strategy using QRISK2 below the threshold would produce a very similar outcome to the use of QRISK2 at all ages, and thus would be similar in cost effectiveness – though with perhaps a small amount of inefficient over- of those who were above the age threshold but had a relatively low level of risk due to having no other risk factors – but it would have the downside of being a more complicated approach. Quality of evidence Framingham is based on a (the gold standard), but in the USA. Inter- exists in the 6 studies that validate Framingham-Anderson (1991) equation in the UK. Calibration data are only available for 3 studies.
Calibration is updated about every 3 years on the basis of a US, but would also need to be re-calibrated specifically for the UK. QRISK2 is derived in the UK from a large database of GP records. There is a large amount of missing data that is dealt with in development of the tool by imputation. QRISK 2 has been externally validated in another UK population. QRISK2 is updated every year. QRISK2 performs better than Framingham in terms of AUC, R 2, D statistics and Brier score and is also better calibrated to UK CVD event rates. Other considerations Other risk assessment tools In their discussion, the GDG considered tools that had external validation in England and Wales.
ASSIGN was developed in Scotland as part of the Scottish CV study. It is similar to QRISK2 and it includes the similar risk factors but with slightly different weighting coefficients. The GDG decided not to consider this tool because the deprivation score uses postcodes specific to Scotland with no easy method to correlate these with the England and Wales population.
During the development of the guideline the British Societies (JBS) published consensus recommendations for the prevention of cardiovascular disease. This includes a tool based on QRISK Lifetime. The JBS3 recommendations are to treat people with lifestyle advice and drugs according to their 10 year absolute risk and to use the lifestyle risk tool for information and education particularly in people whose risk is lower than the threshold for drug.
Lifetime risk versus 10-year risk The GDG considered that lifetime risk and 10-year risk tools exist for both Framingham and QRISK2. The different versions identify different populations as being at risk. The GDG reviewed the evidence and the statistical techniques used to validate the performance of different risk tools. The GDG considered that lifetime risk tools should not be considered. Expert advice was that there are technical methodological issues with how to derive, validate and present prognostic quantification of the outputs of these tools compared with the outputs of 10-year risk tools. Ten-year risk was also considered more relevant to whose risk could most profitably be reduced by any and in particular when prescribed drug should start.
Threshold for This guideline recommends risk assessment for the introduction of modification but other guidelines also cross-refer to this guideline, for example (CG127). At the time the clinical review was carried out, the threshold for for modification was not known. The guideline recommends deciding on drug in people with stage 1 if the 10-year CVD risk is 20% or more. The review reported on metrics at risks of 5%, 10%, 15% and 20% where available, however, the majority of the evidence reported sensitivity and specificity of the tools at 15%, 20% and 30%.
Following the health economics modelling, the GDG have chosen 10% 10-year CV risk as measured by QRISK2 as the threshold for offering drug. None of the included studies reported data on this specific threshold; only one study (Wald 2011), based on a simulated population, reported sensitivity and specificity using thresholds of 8% and 5% CV risk as measured by Framingham-Anderson, concluding that at these thresholds the performance of Framingham is comparable to an assessment strategy based on age alone, with cut-off ages of 55 years and 50 years respectively.
Age screening The GDG had requested information on age screening as part of this review. They acknowledged that since age is the most important contributor to CVD risk, an age-alone strategy would identify most people at risk. The GDG were concerned however that an age-alone strategy would not allow identification of people with increased risk at a younger age whose risk is increased by ethnicity, comorbidity or lifestyle factors. Younger people will also gain from over a longer time period. The only evidence available for age is from a simulated.
The GDG considered it worthwhile to develop a research recommendation to use a to compare age and other simplified methods of risk assessment with validated risk tools. QRISK 2 has an upper limit of 84 years.
All people of 85 years and older are at high risk of CVD by virtue of age alone. Decisions about should be made on a clinical basis according to proposed and other factors such as comorbidities and patient choice. QRISK2 and Framingham derivation One of the disadvantages of QRISK2 is that the databases from which it is developed will include people already on drug such as. The Framingham are more representative of people in whom has not yet been initiated. Framingham will therefore overestimate observed risk in a modern population yet may provide better information on risk before any is initiated. Ease of use of QRISK2 and Framingham As the risk tools are to be widely used, it is essential that both are easily available to potential users. The GDG noted that both tools are available electronically in GP practices and as web applications for other users.
Frequency of risk assessment The GDG discussed whether it was appropriate to recommend how often risk assessment should be carried out. Risk assessment is currently mandated to be performed every 5 years as part of the NHS Health Check programme. The most significant CVD risk factor driving any transition to using a risk tool is age. While multiple determinations of individual CVD risk factors at any single time point improve the accuracy of risk assessment, repeated risk assessments (such as annual checks) are not likely to be clinically useful given the errors involved in the process. Any significant changes in or knowledge of might necessitate a repeat of risk assessment.
Recommendation 9. Do not use a risk assessment tool to assess CVD risk in people with. See recommendations 59, 60 and 61 for advice on with statins for people with type 1 diabetes.
new 2014 This recommendation updates and replaces recommendation 1.10.1.2 from (NICE clinical guideline 15). Relative values of different outcomes The clinical outcomes that the GDG wished to predict were CV events, in particular CV mortality, non-fatal MI and. The GDG considered calibration, discrimination and reclassification of risk assessment tools to be important. The GDG considered that any risk tool should accurately predict the number of individuals likely to have an event, that is it needs to be well calibrated; over- or under- prediction would lead to over- or under-, which could result in significant harm. Discrimination is important to correctly classify individuals into risk groups to inform decisions on pharmacological. The GDG noted that reclassification indices are being used in comparing the performance of different risk tools around decision thresholds. The reclassification index is the difference between people re-classified to high risk or low risk, but it can be calculated in different ways and the absolute magnitude of changes is relevant as well as the difference.
There is lack of agreement on the definition of reclassification index. The clinical reclassification index, based on clinically relevant re-classification decisions should also be considered.
No suitable risk assessment outcome tool was identified for CV events in in a UK population. Trade-off between clinical benefits and harms One purpose of risk assessment is to decide on suitability for.
Over-prediction will result in unnecessary and, whereas under-prediction means a person would not be offered potentially preventative. The GDG considered that the use of an appropriate assessment tool is unlikely to harm an individual patient. No evidence was found on the development of a specific substantially validated CV risk assessment tool for people with in a UK population. Economic considerations No economic evidence was identified relating to people with. Unless the use of a different tool requires different resource use in terms of numbers of appointments or carried out, which does not appear to be the case, the cost effectiveness of using a risk assessment tool will be largely related to its effectiveness in correctly predicting risk and so minimising over- and under-.
As the effectiveness of risk tools in this population is unknown, it is not possible to judge the cost effectiveness of using such tools in this population. Quality of evidence No evidence was found for the population; the recommendation is based on GDG expert opinion and consensus. Other considerations The GDG noted that CV risk is elevated in epidemiological and of patients with.
This has been confirmed in a population that included UK patients. Clinically type 1 and are different conditions. Epidemiological studies show a different rank-order for the significance of individual CV risk factors in type 1 and. In addition the evidence that exists in is mostly based on surrogate outcome measures of rather than large scale CV event data. These studies identify features of the as highly relevant to the occurrence of CV events in and consistently identify waist-hip ratio allied with and (also non-) as significant risk factors. The GDG considered that specialists in will recognise these risk factors and treat people accordingly.
QRISK2 does include a tick box for. This however provides just a yes/no answer and does not include factors considered clinically important such as length of time patient has had. The GDG noted that there is no validation or calibration data regarding how QRISK2, or any other risk tool, performs for people with. The GDG concluded that no risk assessment tool could be applied to patients with type I but that they are likely to meet clinical criteria for having a CV risk substantially in excess of the general population of the same age and gender. The GDG considered it useful to cross-refer to the recommendations on with statins in people with.
Recommendation 10. Use the QRISK2 risk assessment tool to assess CVD risk in people with.
new 2014 This recommendation updates and replaces recommendations 1.9.1 – 1.9.3 from (NICE clinical guideline 87). Relative values of different outcomes The clinical outcomes that the GDG wished to predict were CV events, in particular CV mortality, non-fatal MI and.
The GDG considered calibration, discrimination and reclassification of risk assessment tools to be important. The GDG considered that any risk tool should accurately predict the number of individuals likely to have an event, that is it needs to be well calibrated; over- or under- prediction would lead to over- or under-, which could result in significant harm. Discrimination is important to correctly classify individuals into risk groups to inform decisions on pharmacological. The GDG noted that reclassification indices are being used in comparing the performance of different risk tools around decision thresholds. The reclassification index is the difference between people re-classified to high risk or low risk, but it can be calculated in different ways and the absolute magnitude of changes is relevant as well as the difference.
There is lack of agreement on the definition of reclassification index. The clinical reclassification index, based on clinically relevant re-classification decisions should also be considered. Trade-off between clinical benefits and harms One purpose of risk assessment is to decide on suitability for.
Over-prediction will result in unnecessary and, whereas under-prediction means a person would not be offered potentially preventative. The evidence indicated that all the tools considered are better than chance at predicting risk. The GDG considered that the use of an appropriate assessment tool is unlikely to harm an individual patient but were concerned that emphasis on a risk assessment tool might distract from the need to use clinical judgement to inform interpretation of the tool according to the circumstances of each individual patient. Economic considerations No economic evidence was identified relating to people with. Unless the use of a different tool requires different resource use in terms of numbers of appointments or carried out, which does not appear to be the case, the cost effectiveness of using a risk assessment tool will be largely related to its effectiveness in correctly predicting risk and so minimising over- and under. As the QRISK2 risk engine is felt to be likely to be the most clinically appropriate tool it is also likely to be cost effective compared to any other option.
Quality of evidence Three studies carried out head-to-head comparisons of UKPDS versus Framingham, and the quality of the evidence ranged from low to high risk of. The UKPDS is based on a historical and has not been updated. QRISK2 has the option to select as risk factor. The derivation and external validation of QRISK2 studies are at high risk of. Although there are no external validation studies of QRISK2 in the population, the development of QRISK2 includes more than 40,000 patients with prevalent within primary care, compared to the 4540 patients newly diagnosed with that form the UKPDS derivation. Other considerations Multiple epidemiological and the evidence review of studies have established that CVD event rates are increased in patients with compared with the general population.
Epidemiological studies of CV risk in have shown a strong relationship with and non. The GDG discussed the concept of CVD risk equivalence in people with. This is the idea that risk in people with is elevated to the same extent that risk is elevated in people who have evidence of CVD. The GDG considered that the risk is not quite as high as in people being treated for secondary prevention and that use of a risk tool should be considered for the populations. The GDG considered that QRISK2 is updated annually and takes into account the changing of CVD risk factors such as. It is also in common usage across the NHS and well integrated into the GP computer systems.
The use of the same risk tool in people without and people with who are being treated for primary prevention will aid implementation of risk screening strategies. Recommendation 11. Do not use a risk assessment tool to assess CVD risk in people with an estimated (eGFR) less than 60 ml/min/1.73 m 2 and/or albuminuria. These people are at increased risk of CVD. See recommendation 62 for advice on with statins for people with. new 2014 Relative values of different outcomes The clinical outcomes that the GDG wished to predict were CV events, in particular CV mortality, non-fatal MI and.
The GDG considered calibration, discrimination and reclassification of risk assessment tools to be important. The GDG considered that any risk tool should accurately predict the number of individuals likely to have an event, that is it needs to be well calibrated; over- or under- prediction would lead to over- or under-, which could result in significant harm. Discrimination is important to correctly classify individuals into risk groups to inform decisions on pharmacological. The GDG noted that reclassification indices are being used in comparing the performance of different risk tools around decision thresholds. The reclassification index is the difference between people re-classified to high risk or low risk, but it can be calculated in different ways and the absolute magnitude of changes is relevant as well as the difference.
There is lack of agreement on the definition of reclassification index. The clinical reclassification index, based on clinically relevant re-classification decisions should also be considered. Trade-off between clinical benefits and harms One purpose of risk assessment is to decide on suitability for. Over-prediction will result in unnecessary and, whereas under-prediction means a person would not be offered potentially preventative.
The evidence indicated that all the tools considered are better than chance at predicting risk. The GDG considered that the use of an appropriate assessment tool is unlikely to harm an individual patient but were concerned that emphasis on a risk assessment tool might distract from the need to use clinical judgement to inform interpretation of the tool according to the circumstances of each individual patient. Economic considerations No economic evidence was identified relating to people with CKD.
Unless the use of a different tool requires different resource use in terms of numbers of appointments or carried out, which does not appear to be the case, the cost effectiveness of using a risk assessment tool will be largely related to its effectiveness in correctly predicting risk and so minimising over- or under. As the QRISK2 tool is felt to be likely to be the most clinically appropriate tool it is also likely to be cost effective compared to any other option.
Quality of evidence No evidence was found specific to the CKD population; the recommendations are based on GDG consensus and expert opinion. Other considerations The GDG were joined by a -opted expert in for discussion of assessment of risk and of people with CKD. The GDG agreed that people with a significant degree CKD are at increased CVD risk based on epidemiological studies and the event rate data for the subgroups with renal impairment in the evidence review of populations. CV death in later stages of is however likely to be related to non-atherosclerotic disease such as. The classification of CKD is complicated. The NICE guideline on suggests that people with eGFR greater than 60mls/min/1.73m 2 but without albuminuria should not be considered to have as they do not have evidence of damage.
However those with albuminuria are considered to have CKD whatever their eGFR and are at increased risk of progressing to more severe. The presence of albuminuria is also associated with increased risk of CVD when albuminuria is greater than 3mg/ mmol creatinine. The GDG noted that QRISK2 does provide a tick box for “CKD”. This however is potentially misleading because it does not distinguish amongst grades of eGFR and albuminuria and includes under this heading quite different renal pathological processes that could generically be called ‘’, for example.
Framingham Score Risk Factors
People with albuminuria or with eGFR. Recommendations 12. Complete as many fields of the risk assessment tool as possible. new 2014 13. Routinely record ethnicity, body mass index and of premature CVD in medical records. Consider socioeconomic status as an additional factor that contributes to CVD risk. Do not use a risk assessment tool for people with pre-existing CVD.
2008, amended 2014 16. Do not use a risk assessment tool for people who are at high risk of developing CVD because of familial (see NICE clinical guideline 71) or other inherited disorders of. 2008, amended 2014 17. When using the risk score to inform drug decisions, particularly if it is near to the threshold for treatment, take into account other factors that:. People with such as, and other systemic inflammatory disorders.
2008, amended 2014 19. Recognise that CVD risk will be underestimated in people who are already taking or modification, or who have recently stopped smoking. Use clinical judgement to decide on further of risk factors in people who are below the CVD risk threshold for treatment. 2008, amended 2014 20. Severe (body mass index greater than 40 kg/m 2) increases CVD risk.
Take this into account when using risk scores to inform decisions in this group (see NICE clinical guideline 43). Consider people aged 85 or older to be at increased risk of CVD because of age alone, particularly people who smoke or have raised.
2008, amended 2014. Why this is important Current risk assessment tools rely on a complex set of data derived from demographic, lifestyle, physiological and biochemical parameters. The principal determinant of CVD risk is age, and this may be sufficient to identify high-risk populations. However, focusing on age alone may result in people being missed who are at higher risk as a result of other factors that do not require access to intensive resources, such as smoking status, and deprivation.
It is important therefore to assess age against validated simplified and complex CVD risk tools in prediction of people at high risk.